- Home
- Solutions
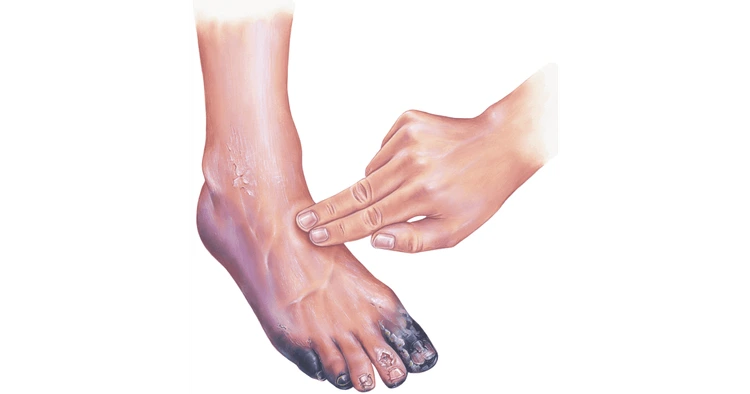
- Foot care & Diabetic Solution
- Gangrene treatment
- wound care and supportive therapy
wound care and supportive therapy
wound care and supportive therapy
Table of Content
2. Wound Care Management
3. Wound Healing Process & Best Practices
4. Advanced & Specialized Wound Care
5. Conclusion of Wound Care
6. Introduction to Supportive Therapy
7. Types of Supportive Therapy
8. Supportive Therapy in Various Conditions
9. Benefits of Supportive Therapy
10. Conclusion of Supportive Therapy
11. Conclusion
12. Faqs
Introduction of Wound Care
Wound care is one of the most essential aspects of modern healthcare. At its core, wound care refers to the process of cleaning, treating, and protecting wounds to promote faster and safer healing. Whether it’s a minor cut, a surgical incision, or a chronic diabetic ulcer, every wound demands the right attention to prevent infections and long-term complications.
The meaning of wound care goes beyond applying a simple bandage. It involves understanding the type of wound, assessing its depth and severity, and applying the correct dressing or treatment. From minor abrasions to complex post-operative wounds, appropriate wound management ensures optimal tissue repair and reduces scarring.
The importance of wound care lies in its ability to prevent infections, minimize pain, and restore function. Neglecting proper care can lead to delayed healing, sepsis, or even chronic wounds that may require surgical intervention. For instance, diabetic patients who ignore small foot wounds often face complications like ulcers or amputations.
There are various types of wound care, including:
- Basic wound care: Cleaning and dressing minor wounds.
- Surgical wound care: Managing post-surgery incisions and stitches.
- Chronic wound care: Treating non-healing wounds such as diabetic or venous ulcers.
- Advanced wound care: Using specialized products and therapies like Microdacyn 60, hydrocolloids, or negative pressure therapy for complex wounds.
The wound care procedure typically includes cleaning with antiseptics, removing dead tissue, applying an appropriate dressing, and monitoring the healing progress. Professionals also assess for signs of infection like redness, warmth, swelling, or pus. Each step plays a vital role in reducing the risk of complications and ensuring proper healing. For severe or complex cases, such as gangrene treatment without surgery, specialized wound care approaches are essential to restore tissue health and prevent further damage.
Proper wound care is more than a medical routine—it’s a commitment to health, comfort, and recovery. It’s the bridge between injury and complete healing, and mastering it ensures that patients not only heal but thrive.
Wound Care Management
- Effective wound care management is about combining the right clinical knowledge, techniques, and products to ensure optimal recovery. Every wound has unique needs depending on its type, location, and cause. Managing a surgical wound is completely different from handling a diabetic ulcer or a dog bite. Therefore, understanding various aspects of wound care is essential for both healthcare professionals and patients.
- Let’s start with advanced wound care, which uses modern technologies and products to accelerate healing. This includes hydrocolloid dressings, alginate dressings, foam dressings, and innovative antiseptic solutions such as Microdacyn 60 wound care—a brand known for its antimicrobial properties and tissue-friendly formulation. Advanced wound care helps reduce infection, control exudate, and create an ideal moist environment for tissue regeneration.
- Wound care after surgery is a crucial phase of post-operative recovery. Surgical wounds require careful cleaning and dressing changes to prevent infection. It’s vital to keep the area dry and monitor for signs of inflammation. In cases of surgical wound care, medical professionals often use sterile techniques, absorbent dressings, and topical antiseptics to ensure the incision heals without complications. Patients should also avoid physical strain to prevent reopening of the wound.
- When it comes to surgery wound care, it’s important to remember that even minor negligence can cause severe infections. The skin acts as the body’s first defense barrier; once it’s cut, bacteria can easily enter. That’s why following your doctor’s instructions—such as regular cleaning, applying prescribed ointments, and avoiding touching the wound with unwashed hands—is critical.
- Another important aspect is wound care after staples are removed. Once staples or sutures are taken out, the skin is still fragile. The newly formed tissue must be protected from pressure and moisture. Applying silicone gels or gentle dressings can help prevent hypertrophic scarring and support full recovery.
- Dog bite puncture wound care requires extra caution because animal bites often introduce bacteria deep into the skin. Immediate washing with soap and water, followed by antiseptic application and medical evaluation, is necessary. In some cases, antibiotics or tetanus shots may be prescribed to prevent infection.
- Diabetic ulcer wound care is one of the most challenging forms of wound management. High blood sugar slows healing and increases infection risk. Regular debridement, moisture control, and advanced dressings are used to promote recovery. Foot inspections, blood sugar monitoring, and specialized footwear can also prevent new ulcers from forming.
- Venous ulcer wound care, which overlaps with both wound care and supportive therapy, focuses on improving circulation and reducing swelling. Compression therapy, elevation, and medical-grade dressings are key strategies.
- Lastly, wound care products play an important role in every stage of healing. These include antiseptics, hydrogel dressings, alginates, collagen sheets, and Microdacyn 60 wound care solutions. Using the right product ensures that the wound remains clean, hydrated, and protected against bacteria.
- Proper wound care management is not just about treatment—it’s about prevention, consistency, and education. Knowing when to change dressings, how to prevent infection, and when to seek help can make a life-changing difference in recovery outcomes.
Wound Healing Process & Best Practices
The wound healing process is a fascinating and complex biological journey that our body performs naturally. When an injury occurs, the body immediately activates a series of responses to close the wound, fight infection, and rebuild damaged tissues. However, proper care and best practices can significantly influence how well and how fast a wound heals.
The healing process generally unfolds in four main stages:
- Hemostasis – This is the first stage, where the body immediately stops bleeding by forming a clot.
- Inflammation – The area may become red, warm, and swollen as white blood cells work to remove bacteria and debris.
- Proliferation – New tissue begins to form, covering the wound with fresh skin cells and collagen.
- Maturation (Remodeling) – The final stage where the wound strengthens, and the scar gradually fades over time.
Each of these phases requires the right wound care procedure to support healing. For example, cleaning with antiseptics, using sterile dressings, and avoiding unnecessary pressure are crucial steps. A wound that is not cleaned or protected properly may become infected, delaying the healing process.
Preventing Infection
Infection prevention is the cornerstone of successful wound healing. Even a small cut can become dangerous if bacteria invade the area. To prevent infection:
- Always wash your hands before and after touching the wound.
- Clean the wound gently with a mild antiseptic solution or saline.
- Use sterile dressings and change them regularly.
- Avoid using harsh chemicals like hydrogen peroxide unless prescribed.
- Watch for signs of infection such as redness, warmth, pus, or fever.
Microdacyn 60 wound care has become a preferred antiseptic for many professionals due to its ability to destroy harmful microorganisms without damaging healthy tissue. It’s gentle enough for chronic wounds but powerful enough to protect against infection.
When to Seek Medical Help
Not all wounds can be managed at home. You should seek professional care if:
- The wound is deep, large, or bleeding continuously.
- There’s a sign of infection or pus.
- The wound doesn’t start healing after a week.
- It’s caused by an animal or human bite.
- You have diabetes or a compromised immune system.
Delaying treatment can result in complications like cellulitis, abscess formation, or chronic ulcers. Medical professionals can assess the wound depth, prescribe antibiotics if needed, and recommend specialized dressings or therapies.
Role of Nutrition & Oxygen Therapy in Wound Healing
Healing doesn’t depend on external care alone—your body needs the right nutrition and oxygen to repair itself. Protein, vitamin C, zinc, and iron are key nutrients that support collagen formation and immune defense. Dehydration or malnutrition can delay healing, especially in elderly or diabetic patients.
Oxygen therapy plays an equally crucial role. Hyperbaric Oxygen Therapy (HBOT), for example, delivers 100% oxygen under pressure, which enhances tissue repair, fights infection, and speeds up recovery. Oxygen helps generate new blood vessels, especially in chronic wounds where circulation is poor.
By combining proper cleaning, infection prevention, nutritional support, and modern wound care products, you give your body the best possible chance to heal efficiently and safely.
Advanced & Specialized Wound Care
As medical science evolves, advanced and specialized wound care techniques are transforming the way chronic and complex wounds are treated. Gone are the days when simple bandages were the only solution. Today, a wide range of innovative therapies—like Negative Pressure Wound Therapy (NPWT), Hyperbaric Oxygen Therapy (HBOT), and even maggot therapy—are available to accelerate healing and reduce infection risks.
Advanced Wound Care Techniques
One of the most popular modern treatments is Negative Pressure Wound Therapy (NPWT). This method involves placing a sealed dressing over the wound and connecting it to a vacuum pump. The gentle suction removes excess fluid and bacteria, increases blood flow, and stimulates new tissue growth. It’s particularly effective for surgical wounds, pressure ulcers, and diabetic ulcers.
Hyperbaric Oxygen Therapy (HBOT) is another powerful treatment option. In HBOT, patients breathe pure oxygen in a pressurized chamber. This process allows more oxygen to dissolve into the bloodstream, promoting tissue repair, reducing swelling, and killing bacteria. Chronic non-healing wounds, such as those caused by diabetes or radiation injury, benefit greatly from this therapy.
Then there’s maggot therapy, which might sound unusual but has remarkable healing potential. Sterile larvae are placed on the wound to consume dead tissue, disinfect the wound, and speed up healing. They release enzymes that selectively break down necrotic tissue without harming healthy skin—a natural, effective form of debridement.
Chronic Wound Care
Chronic wounds are those that fail to heal after several weeks of standard treatment. Conditions like diabetic ulcers, venous ulcers, and pressure sores fall under this category. Chronic wound management requires a multidisciplinary approach involving doctors, nurses, nutritionists, and sometimes surgeons.
For instance, diabetic ulcer wound care requires strict blood sugar control, specialized dressings, and sometimes offloading devices to reduce pressure on the affected area. Meanwhile, venous ulcer wound care often includes compression therapy and elevation of the legs to improve circulation. Pressure ulcers—common among bedridden patients—demand regular repositioning, moisture management, and cushioning.
Microdacyn 60 wound care also plays an important role in managing chronic wounds. Its hypochlorous acid formula helps kill pathogens while supporting tissue regeneration, making it suitable for delicate skin and long-term treatment.
New Trends and Innovations in Wound Care
The field of wound management continues to evolve with biotechnology and regenerative medicine leading the way. Some of the latest trends include:
- Bioengineered skin substitutes that mimic real skin to cover large wounds.
- Stem cell therapy to regenerate damaged tissues.
- Smart dressings that change color when infection is detected.
- Nanotechnology-based ointments that deliver targeted antimicrobial effects.
The integration of AI and digital monitoring systems has also made it easier to track wound progress. Remote wound assessment through smart devices allows healthcare providers to make informed decisions without requiring frequent clinic visits.
In short, advanced wound care is a blend of technology, science, and compassion. It not only speeds up recovery but also improves the quality of life for patients with severe or chronic wounds. With each innovation, the gap between injury and complete healing becomes smaller.If you or a loved one are facing emergency symptoms related to diabetic foot complications or gangrene, don’t wait—contact us immediately for prompt, compassionate intensive care and support.
Conclusion of Wound Care
The journey of wound care doesn’t end once the wound closes—it continues through ongoing monitoring, maintenance, and education. Proper wound care is about prevention as much as it is about treatment. Whether you’re managing a small surgical incision or a chronic diabetic ulcer, the right practices can make the difference between quick healing and prolonged suffering.
Summary of Effective Wound Care Management
Effective wound care is a comprehensive process that involves several layers of attention. It starts with accurate assessment—understanding the type and depth of the wound. From there, choosing the correct wound care products such as antiseptics, hydrocolloids, and antimicrobial dressings like Microdacyn 60 helps create the ideal healing environment.
Regular cleaning, infection prevention, and consistent dressing changes are vital. For surgical wounds, maintaining sterility is the top priority. For chronic wounds, managing underlying conditions such as diabetes or venous insufficiency is equally important.
It’s also crucial to follow up with your healthcare provider. Even when wounds appear healed externally, internal tissues may still be fragile. Regular medical checkups and adherence to post-care instructions ensure complete recovery and reduce the risk of recurrence.
Importance of Proper Aftercare
Aftercare is often the most overlooked part of wound management. However, it’s during this stage that the wound strengthens and tissues rebuild. Simple habits—like keeping the area moisturized, avoiding unnecessary friction, and protecting from UV exposure—help minimize scarring and discoloration.
Patients recovering from surgery wound care or staple removal should avoid strenuous movements that can reopen the incision. For chronic wounds like diabetic or venous ulcers, continuous preventive measures are essential—proper footwear, compression therapy, and good hygiene can save patients from repeated infections.
Nutrition plays a silent yet vital role here. Foods rich in vitamin A, vitamin C, zinc, and protein help in collagen formation and tissue repair. Hydration also supports skin elasticity and faster healing.
Long-Term Wound Care Maintenance
Long-term wound care isn’t just about healing—it’s about protecting the body from future injuries. Regular skin checks, early treatment of cuts, and proper management of chronic diseases form the foundation of preventive wound care.
In healthcare facilities, adopting a standardized wound care protocol ensures that patients receive consistent and evidence-based treatment. Education is key—both patients and caregivers should be trained on cleaning techniques, recognizing signs of infection, and using appropriate dressings.
Ultimately, the conclusion of wound care teaches us one lesson: healing is not a race but a process. With attention, patience, and modern innovations, even the most complex wounds can heal effectively.
Introduction to Supportive Therapy
While wound care focuses on physical healing, supportive therapy plays a broader role in maintaining overall well-being and improving quality of life during treatment for various health conditions. It’s the helping hand that manages symptoms, reduces complications, and strengthens patients emotionally and physically as they undergo medical treatments.
Supportive Therapy Meaning
In simple terms, supportive therapy refers to all treatments designed to relieve symptoms and enhance comfort rather than directly curing the underlying disease. It is often used alongside primary or curative therapy to make the healing journey smoother and more bearable.
For instance, a cancer patient receiving chemotherapy may experience fatigue, nausea, or pain. Supportive therapy in this case might include pain management, nutritional support, or counseling to ease these side effects.
Role and Importance in Medical Treatment
Supportive therapy holds immense importance in modern medicine. It bridges the gap between disease management and patient comfort. Whether it’s maintaining hydration in typhoid fever, reducing tremors in neurological disorders, or easing discomfort after surgery, supportive therapy ensures that patients recover not only physically but also mentally.
Doctors often emphasize that supportive care doesn’t replace curative treatments—it complements them. By managing symptoms and preventing secondary complications, supportive therapy allows primary treatments to work more effectively.
Difference Between Curative and Supportive Therapy
The main distinction lies in their goals:
- Curative therapy aims to eliminate the disease entirely.
- Supportive therapy focuses on managing symptoms and improving quality of life.
For example, antibiotics for typhoid fever are curative, while fluid replacement and fever management form the supportive therapy. Similarly, in lung cancer, chemotherapy targets the tumor (curative), whereas supportive therapy helps manage fatigue, nausea, and pain.
In short, supportive therapy is the unsung hero of healthcare—quietly working behind the scenes to make sure patients can endure their treatments and recover with dignity.
Types of Supportive Therapy
Supportive therapy is not a one-size-fits-all approach—it varies widely depending on the patient’s condition, medical history, and overall treatment goals. From dental maintenance to complex disease management, supportive therapy is designed to improve comfort, control symptoms, and enhance recovery. Let’s explore some of the major types and their applications in healthcare.
Supportive Periodontal Therapy
Supportive periodontal therapy (SPT) is a specialized dental treatment aimed at preventing the recurrence of gum disease after initial therapy. Once periodontal disease is brought under control, ongoing maintenance is crucial to keep the gums healthy and prevent bone loss.
SPT typically includes:
- Regular dental cleaning and plaque removal
- Monitoring gum pockets and inflammation
- Guidance on oral hygiene and diet
- Use of antiseptic mouth rinses or medicated gels
This type of therapy highlights how supportive treatment doesn’t always mean managing serious illnesses—it can also involve maintaining results after a successful procedure. Regular supportive periodontal care ensures long-term oral health and minimizes the risk of tooth loss.
Venous Ulcer Supportive Therapy
Venous ulcer supportive therapy overlaps both with wound care and chronic disease management. These ulcers are caused by poor blood flow in the veins, often in the legs. Supportive therapy focuses on reducing swelling, improving circulation, and preventing infection.
Key supportive measures include:
- Compression therapy: Special stockings or wraps to boost venous return
- Leg elevation: Helps reduce swelling and pain
- Proper wound dressing: Keeps the wound clean and moist for optimal healing
- Physical activity: Light exercises to improve circulation
Venous ulcer supportive therapy is a continuous process that requires lifestyle changes along with medical care. Properly managed, it not only promotes wound healing but also prevents recurrence—a crucial part of long-term recovery.
General Supportive Therapy Procedures
Supportive therapy can involve a broad range of treatments that provide comfort and stability during illness. These may include:
- Pain control: Using analgesics or nerve blocks to manage chronic or acute pain
- Fluid therapy: Ensuring hydration and electrolyte balance, especially in fevers or infections
- Nutritional support: Tailoring diets to provide essential vitamins, minerals, and proteins for recovery
- Psychological support: Counseling, therapy, or group support to handle emotional stress
Each of these plays a critical role in comprehensive patient care. For example, in hyponatremia supportive therapy, fluid restriction and electrolyte correction help restore balance without causing complications.
Supportive therapy is not limited to hospitals—it’s often part of home-based care, rehabilitation centers, and chronic illness management programs. By focusing on the whole person, supportive therapy helps patients feel cared for, empowered, and involved in their healing journey.
Supportive Therapy in Various Conditions
The beauty of supportive therapy lies in its adaptability. It can be applied to almost every medical condition—from cancer and infections to hormonal and neurological disorders. Below are some examples of how supportive therapy complements treatment in different health conditions.
Lung Cancer Supportive Therapy
Lung cancer supportive therapy helps patients manage the side effects of chemotherapy, radiation, or surgery. Common supportive treatments include:
- Oxygen therapy to ease breathing
- Pain management using opioids or nerve blockers
- Nutritional support for maintaining weight and strength
- Psychological counseling to cope with emotional stress
These interventions don’t cure cancer but make treatment more tolerable, allowing patients to maintain their quality of life.
Typhoid Fever Supportive Therapy
In typhoid fever, the main treatment is antibiotics. However, supportive therapy plays a vital role in symptom management. It includes:
- Adequate hydration through oral rehydration salts (ORS) or IV fluids
- Antipyretics to control fever
- Nutritional support to restore strength and prevent dehydration
This therapy ensures that the patient’s body remains strong enough to respond effectively to antibiotics and recover faster.
Gynecomastia Supportive Therapy
Gynecomastia supportive therapy helps men deal with the physical and psychological impact of hormonal imbalance leading to breast tissue enlargement. Supportive care may involve counseling, hormone therapy adjustment, and post-surgical care (if surgery is performed). Emotional support is a major component here, as self-image issues often accompany this condition.
Hernia Supportive Therapy
For hernia supportive therapy, pain relief, abdominal support belts, and lifestyle modifications like avoiding heavy lifting or constipation are essential. Post-surgical supportive care focuses on wound healing, preventing infection, and gradually rebuilding abdominal strength.
Hyponatremia Supportive Therapy
In hyponatremia supportive therapy, the main goal is to safely correct low sodium levels without causing complications. This involves fluid management, electrolyte replacement, and sometimes medications that control water retention. Continuous monitoring ensures the patient’s sodium levels are restored at a safe rate.
Telogen Effluvium Supportive Therapy
Telogen effluvium, a temporary hair loss condition caused by stress or hormonal imbalance, benefits from supportive treatments like nutritional supplements, stress reduction, and topical serums to stimulate regrowth. This therapy focuses on restoring scalp health and addressing underlying triggers.
Essential Tremor Supportive Therapy
For neurological disorders such as essential tremor, supportive therapy may include physiotherapy, adaptive devices, and medications to control muscle movement. Emotional and occupational support helps patients continue daily activities confidently.
Benign Prostatic Hyperplasia Supportive Therapy
Benign prostatic hyperplasia (BPH) supportive therapy aims to relieve urinary symptoms and improve bladder function. Alongside medications, supportive strategies include fluid management, bladder training, and dietary adjustments. Post-surgery, wound care and infection prevention are crucial components.
Pityriasis Rosea Supportive Therapy
In pityriasis rosea, a skin condition marked by rashes, supportive therapy includes soothing lotions, antihistamines for itching, and sunlight exposure in moderation. The goal is to ease discomfort and support natural recovery since the condition usually resolves on its own.
Across all these conditions, supportive therapy acts as the invisible yet indispensable partner of medical treatment—helping the body and mind work together toward complete healing.
Benefits of Supportive Therapy
Supportive therapy has become an essential part of modern healthcare because it focuses on the human side of healing. While curative treatments target the disease itself, supportive therapy addresses everything else—the pain, fatigue, anxiety, and side effects that can make recovery difficult. Its goal is to improve not only survival but also comfort and overall quality of life.
Let’s explore the key benefits of supportive therapy that make it a vital complement to traditional medical treatments.
1. Improves Quality of Life
One of the most significant benefits of supportive therapy is its ability to enhance a patient’s daily life during treatment. Chronic illnesses, surgeries, or long-term medications can often leave patients feeling weak and discouraged. Supportive therapy intervenes to help them live more comfortably.
For example, cancer patients receiving chemotherapy may experience nausea, pain, and fatigue. Through supportive therapy—such as nutritional counseling, physiotherapy, and emotional support—they can regain strength, appetite, and hope. Similarly, patients recovering from surgery benefit from wound care support and physical rehabilitation to regain mobility.
Quality of life isn’t just about physical comfort; it’s also about mental and emotional well-being. By addressing both, supportive therapy helps patients maintain dignity and independence during challenging times.
2. Reduces Symptoms and Side Effects
Many medical treatments, while effective, come with side effects. Supportive therapy focuses on minimizing these effects to ensure treatment adherence and success.
Examples include:
- Using pain management techniques for post-surgical or cancer-related discomfort.
- Administering anti-nausea drugs during chemotherapy.
- Offering hydration and electrolyte therapy during typhoid fever.
- Providing hormone balance and emotional support in gynecomastia.
By controlling symptoms, patients can continue their primary treatments without unnecessary interruptions or suffering. Supportive therapy acts like a cushion, softening the harsh impact of aggressive medical interventions.
3. Prevents Complications
Supportive therapy also plays a preventive role. When the body is under stress from illness or treatment, complications can easily arise. Through proper care—such as wound cleaning, nutritional monitoring, or mobility support—patients can avoid infections, pressure ulcers, dehydration, or malnutrition.
In wound care supportive therapy, for instance, preventing infection is paramount. Using Microdacyn 60 wound care or advanced dressings helps stop bacteria before they can cause deeper damage. Similarly, in conditions like hyponatremia, careful monitoring and fluid management prevent life-threatening complications like brain swelling.
Prevention is often more effective—and less costly—than cure. That’s why supportive therapy is increasingly prioritized in hospitals, rehabilitation centers, and even home-care programs.
4. Enhances Recovery and Patient Comfort
Perhaps the most rewarding aspect of supportive therapy is its ability to accelerate recovery. By managing discomfort and keeping the body in balance, it creates the perfect internal environment for healing. Adequate sleep, good nutrition, mental peace, and proper wound management all work together to speed up recovery.
Moreover, supportive therapy restores confidence. When patients feel supported—physically, emotionally, and psychologically—they are more likely to stay motivated and engaged in their recovery process. This holistic approach doesn’t just heal the body; it strengthens the spirit.
In a world where healthcare can sometimes feel mechanical, supportive therapy brings compassion back into the equation. It reminds us that true healing involves both science and empathy.
Conclusion of Supportive Therapy
Supportive therapy is the heart of comprehensive healthcare. It bridges the gap between medical treatment and emotional recovery, ensuring that patients don’t just survive but truly live well through and beyond their illnesses.
Summary of Its Role in Overall Healthcare
- In today’s medical landscape, supportive therapy stands alongside curative treatment as an equal partner. From lung cancer supportive therapy that reduces pain and anxiety to venous ulcer supportive therapy that promotes wound healing, its role is indispensable. It keeps patients strong, hydrated, nourished, and mentally balanced so that their bodies can respond better to primary treatments.
- Whether it’s supportive therapy for typhoid fever to maintain hydration or essential tremor supportive therapy to control involuntary movements, every form of supportive care serves a common purpose—to ease suffering and improve well-being.
Conclusion
The combination of Wound Care & Supportive Therapy represents the foundation of compassionate, effective healthcare. While wound care focuses on restoring the body’s physical integrity, supportive therapy ensures comfort, strength, and emotional balance throughout the healing process.
Together, they provide a comprehensive system that promotes faster recovery, prevents complications, and enhances overall well-being. From managing surgical wounds with Microdacyn 60 to offering comfort during cancer therapy, these approaches work harmoniously to deliver true healing.
Healthcare is not just about curing diseases — it’s about caring for people. And through the science of wound management and the empathy of supportive therapy, patients are given the best chance not just to heal but to thrive.
For those seeking deeper insights into innovative wound care practices and advanced medical treatments, you can also explore Innayat Medical — a trusted platform dedicated to holistic healing, modern therapies, and patient-centered healthcare solutions.
Discover expert-approved wound care and supportive therapy methods to promote healing, prevent infection, and improve overall recovery naturally.
Enquiry Now